功能区亚型是否影响动静脉畸形手术的预后?(Does eloquence subtype influence outcome following arteriovenous malformation surgery?)
英文简介:
OBJECTIVE Although numerous arteriovenous malformation (AVM) grading scales consider eloquence in risk assessment,none differentiate the types of eloquence. The purpose of this study was to determine if eloquence subtype affects clinical outcome.
METHODS This is a retrospective review of a prospectively collected clinical database of brain AVMs treated with microsurgery in the period from 1997 to 2017. The only inclusion criterion for this study was the presence of eloquence as defined by the Spetzler-Martin grading scale. Eloquence was preoperatively categorized by radiologists. Poor outcome was defined as a modified Rankin Scale (mRS) score 3-6, and worsening clinical status was defined as an increase in the mRS score at follow-up. Logistic regression analyses were performed.
RESULTS Two hundred forty-one patients (49.4% female; average age 33.9 years) with eloquent brain AVMs were included in this review. Of the AVMs (average size 2.7 cm), 54.4% presented with hemorrhage, 46.2% had deep venous drainage, and 17.0% were diffuse. The most common eloquence type was sensorimotor (46.1%), followed by visual (27.0%) and language (22.0%). Treatments included microsurgery alone (32.8%), microsurgery plus embolization(51.9%), microsurgery plus radiosurgery (7.9%), and all three modalities (7.5%). Motor mapping was used in 9% of sensorimotor AVM cases, and awake speech mapping was used in 13.2% of AVMs with language eloquence. Complications occurred in 24 patients (10%). At the last follow-up (average 24 months), 71.4% of the patients were unchanged or improved and 16.6% had a poor outcome. There was no statistically significant difference in the baseline patient and AVM characteristics among the different subtypes of eloquence. In a multivariate analysis, in comparison to visual eloquence, both sensorimotor (OR 7.4, p = 0.004) and language (OR 6.5, p = 0.015) eloquence were associated with poor outcomes. Additionally, older age (OR 1.31, p = 0.016) and larger AVM size (OR 1.37, p = 0.034) were associated with poor outcomes.
CONCLUSIONS Unlike visual eloquence, sensorimotor and language eloquence were associated with worse clinical outcomes after the resection of eloquent AVMs. This nuance in AVM eloquence demands consideration before deciding on microsurgical intervention, especially when numerical grading systems produce a score near the borderline between operative and nonoperative management.
中文简介:
目的:虽然许多动静脉畸形(AVM)分级量表在风险评估中考虑了脑功能区,但没有一个能区分脑功能区的类型。本研究的目的是确定脑功能区亚型是否影响临床结果。
方法:回顾性分析1997 - 2017年显微外科手术治疗脑动静脉畸形的临床资料。本研究的纳入标准是由Spetzler-Martin分级量表定义的脑功能区的存在。术前放射学家对雄辩进行了分类。不良结局定义为改良Rankin评分(mRS) 3-6分,临床状态恶化定义为随访时mRS评分增加。进行Logistic回归分析。
结果:241例(49.4%女性;平均年龄33.9岁),拥有雄辩的大脑AVMs。AVMs平均大小为2.7 cm,出血占54.4%,深静脉引流占46.2%,弥漫性占17.0%。较常见的脑功能区类型是感觉运动(46.1%),其次是视觉(27.0%)和语言(22.0%)。治疗包括单纯显微外科手术(32.8%)、显微外科手术加栓塞(51.9%)、显微外科手术加放射外科手术(7.9%)和全部三种方式(7.5%)。9%的感觉运动AVM病例使用运动映射,13.2%的语言脑功能区AVM病例使用清醒语音映射。并发症24例(10%)。在较后一次随访中(平均24个月),71.4%的患者病情没有改变或好转,16.6%的患者预后较差。不同类型脑功能区的基线患者和AVM特征无统计学差异。在多变量分析中,与视觉脑功能区相比,感觉运动(或7.4,p = 0.004)和语言(或6.5,p = 0.015)脑功能区都与不良结果相关。此外,年龄(或1.31,p = 0.016)和AVM大小(或1.37,p = 0.034)与不良预后相关。
结论:与视觉雄辩术不同,感觉运动和语言雄辩术在切除雄辩性AVMs后的临床效果较差。AVM争论的这种细微差别需要在决定显微外科手术干预之前加以考虑,特别是当数值分级系统在手术和非手术处理之间产生分界时。
脑动静脉畸形(AVMs)是颅内血管病变的异质性组,有许多不同的管理模式,包括观察、显微外科手术、放射外科手术、栓塞,较常见的是联合治疗。为了更好地了解显微外科手术、放射外科手术和栓塞手术后的结果,人们开发了许多不同的分级量表。分级量表用于了解治疗风险和选择患者进行特定治疗。较常用的显微外科分级量表是Spetzler-Martin (SM)量表,该量表根据AVMs的大小、静脉引流和脑功能区,将AVMs分为1至5个等级。
虽然这些等级量表中的大多数都考虑了大脑的脑功能区,但它们都无法区分脑功能区的类型。一个例外可能是基于无线电检测的分级系统,它考虑到了AVM定位,这是脑功能区类型的一个替代。因此,例如,在马达带中有AVM的病人,在光学辐射中可能得到与有AVM的病人相同的等级。这些结构的损伤可能导致不同的神经功能缺陷,对整体临床结果的影响可能是可变的。人们对损伤至脑功能区距离(LED)有的兴趣,但对具体脑功能区类型切除风险的评估尚缺乏研究。本研究的目的是确定脑功能区类型如何影响临床结果。我们假设切除有感觉运动脑功能区的动静脉畸形会比切除有语言、视觉或协调脑功能区的动静脉畸形的临床效果更差。
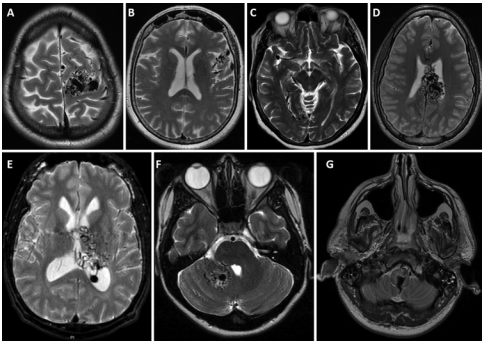
图示:以功能区类型为例的图像:感觉运动(A)、语言(B)、视觉(C)、胼胝体(D)、丘脑(E)、小脑深部核(F)和脑干(G)。
该研究主要人员之一为INC国际神经外科医生集团旗下组织国际神经外科顾问团(WANG)成员Michael T. Lawton 教授。Michael T. Lawton 教授是当今国际上享有盛誉的脑血管病教授,他专注各脑血管病、脑动脉瘤、动静脉畸形、海绵状畸形、血管搭桥、中风、颅底肿瘤的手术治疗,对于较大而复杂的脑动脉瘤手术尤为精通。此外,他还提供中枢、外周和自主神经系统疾病的手术和非手术治疗(即预防、诊断、评估、治疗、重症监护和康复),包括其支持结构和血管供应;评估和治疗改变神经系统功能或活动的病理过程。对于脑紊乱、颅外颈动脉、椎动脉、脑垂体紊乱、脊髓/脑膜和脊柱疾病(包括可能需要通过脊柱融合或器械治疗的疾病)等有丰富经验。目前拥有4400余例脑动脉瘤、800余例动静脉畸形和1000余例海绵状畸形患者的成功治疗经验。




