德国INI国际神经科学研究所在神经外科界享誉国际,擅长对各种神外疾病的手术治疗,是听神经瘤、颅底及脑干疾病方面!德国INI在听神经瘤方面的许多理念、手术术式、术后并发症控制和管理等方面的贡献可谓比比皆是。此篇我们精选汇编了近十余年来其在听神经瘤方面手术的研究。
关键词:家族性纤维瘤病,术后复发性,放疗后复发性,较大型,囊性。
RISIA,神经移植术,面神经重建修复。
1. 乙状窦后内听道上-内扩展硬膜内入路(RISIA)切除累及岩骨的复发性较大听神经瘤:手术技术报告。
Retrosigmoid Intradural Suprameatal-Inframeatal Approach for Complete Surgical Removal of a Giant Recurrent Vestibular Schwannoma with Severe Petrous Bone Involvement: Technical Case Report.
手术切除严重累及岩骨的复发性较大听神经瘤具有严重的并发症风险,手术挑战较大。病例描述:27岁男性患者,较大的听神经瘤复发(4.5cm),肿瘤累及Meckel腔和左岩段颈内动脉。由于肿瘤压迫和先前手术史,症状包括左面部完全麻痹和听力丧失,左侧三叉神经、外展神经麻痹及后组颅神经功能障碍。该患者还表现出严重的不协调和共济失调。经磨除岩骨上-内方部分骨质的RISIA入路,肿瘤得到完全切除,术后未发现相关并发症。术后患者平衡和颅神经功能完全恢复(除面神经和耳蜗神经)。结论:RISIA入路可以顺利、合适地实现完全切除肿瘤,即使是在严重累及Meckel腔和岩段颈内动脉的病例中。这是一个通过RISIA入路成功地完全切除复发性较大听神经瘤的报告。
Surgical removal of giant vestibular schwannomas with severe petrous bone involvement remains challenging due to the high risk of complications. The retrosigmoid intradural suprameatal-inframeatal approach (RISIA) allows for safe exposure extending from Meckel's cave to the petrous internal carotid artery (ICA). CASE DESCRIPTION: A 27-year-old man presented with recurrence of a giant vestibular schwannoma (4.5 cm) invading Meckel's cave and the left petrous ICA. Symptoms included complete left facial palsy and hearing loss due to tumor invasion and previous operations, as well as left-sided trigeminal hypesthesia, abducens nerve palsy, and lower cranial nerve dysfunction due to tumor compression. The patient also exhibited severe discoordination and ataxia. The tumor was completely resected via the RISIA, which involved drilling of the suprameatal and inframeatal portions of the petrous bone. No approach-related complications were observed. Full recovery of cranial nerve functions (with the exception of those related to the facial and cochlear nerves) and balance were observed postoperatively. CONCLUSIONS: The RISIA allows for safe and effective surgical access during complete tumor resection, even when severe involvement of Meckel's cave and the petrous ICA are observed. The present report is the first to demonstrate the usefulness of this approach in patients with recurrent giant vestibular schwannoma.
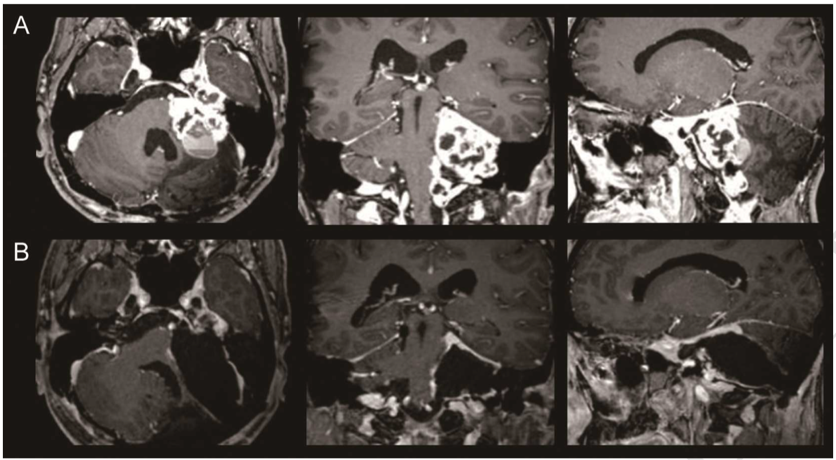
复发性较大听神经瘤经RISIA全切,术前术后MR对比
2. 2型神经纤维瘤病听神经瘤的显微外科治疗:适应症和结果。
Microsurgery management of vestibular schwannomas in neurofibromatosis type 2: indications and results.
目的:分析对2型神经纤维瘤病(NF2)患者的经验和治疗策略,侧重于听神经瘤(VS)手术。方法:在35年的时间里,术者(M.S.)对165例NF2患者进行了手术,手术的VS总数为210。该回顾性分析包括145位手术的患者。分析了病历、手术报告、神经系统检查、听力检查和影像学检查。结果:在85%的病例中实现了肿瘤全切。在15%的患者中,有意次全切是为了听力保护及脑干减压。听神经保留率为35%,当术前患者有合适听力诱发时,听神经保留率为65%,23%患者实现了双侧听神经保留。面神经的解剖保留率为89%。
结论:NF2患者的VS手术目标应该是在不以牺牲神经功能为代价下全切肿瘤,精心的个性化治疗策略有助于延长生存期并保留神经功能。
Aim:To analyze the senior author's experience and strategy of treatment of patients with neurofibromatosis type 2 (NF2), with particular emphasis on vestibular schwannoma (VS) surgery.
MATERIALS AND METHODS: Over a period of more than 35 years, the senior author (M.S.) has operated on more than 165 patients with NF2. The total number of VS surgeries was 210. This retrospective analysis includes 145 consecutively operated patients. Medical records, operative reports, follow-up neurological, audiometric examinations, and neuroradiological findings were analyzed. RESULTS: Total tumor removal was achieved in 85% of the operated tumors. In 15%, deliberately subtotal removal was performed for brain stem decompression and hearing preservation in the only hearing ear. The overall rate of hearing preservation was 35%. When only patients with preserved useful preoperative hearing were included, the rate was 65%. Bilateral hearing after surgery was preserved in 23% of the patients. The anatomical integrity of the facial nerve was preserved in 89%.
CONCLUSIONS: The goal of VS surgery in patients with NF2 should be complete removal but not at the expense of functional impairment. Carefully individualized treatment strategy offers the possibility of prolongation of life and preservation of neurological functions.
3. 听神经瘤术后使用端-侧腓肠神经异位移植术修复面部神经功能:手术技术报告
Using an end-to-side interposed sural nerve graft for facial nerve reinforcement after vestibular schwannoma resection. Technical note.
在过去的30年中,听神经瘤手术后面部和听神经保存率提高了。然而,部分或完全受损的面神经的治疗仍然面临严峻的形势。在这种情况下,可以通过即时或择期手术进行治疗。基于近期成功的端-侧神经吻合术的研究,作者将该技术应用于在听神经瘤手术中面神经解剖保留但功能部分缺损的患者,作者使用端-侧腓肠神经异位移植以增强部分面神经解剖的连续性。术后18个月的随访检查显示,面部神经功能的效果令人满意。在部分面部神经损伤的病例,端-侧神经异位移植是一种合理的修复方式,并且可能是未来其他颅神经损伤的治疗选择。
Increasing rates of facial and cochlear nerve preservation after vestibular schwannoma surgery have been achieved in the last 30 years. However, the management of a partially or completely damaged facial nerve remains an important issue. In such a case, several immediate or delayed repair techniques have been used. On the basis of recent studies of successful end-to-side neurorrhaphy, the authors applied this technique in a patient with an anatomically preserved but partially injured facial nerve during vestibular schwannoma surgery. The authors interposed a sural nerve graft to reinforce the facial nerve whose partial anatomical continuity had been preserved. On follow-up examinations 18 months after surgery, satisfactory cosmetic results for facial nerve function were observed. The end-to-side interposed nerve graft appears to be a reasonable alternative in cases of partial facial nerve injury, and might be a future therapeutic option for other cranial nerve injuries.
4. 放疗术失败后的听神经瘤患者的外科治疗。
Surgical treatment of patients with vestibular schwannomas after failed previous radiosurgery.
越来越多的听神经瘤(VSs)患者接受放疗,但是,据报道有2%9%的患者出现放疗失败-或继发性再生长。在压迫脑干的大肿瘤中以及神经功能快速恶化的患者中,手术切除是合理的治疗选择。方法:作者评估了28例VS患者中先前放疗与手术结果的相关性。该研究进一步细分为A组(术前有过放疗的患者)和B组(术前有过放疗且肿瘤部分切除的患者)。将这两组患者的功能和一般结果与对照组进行比较(无先前治疗的患者)。结果:A组15例,B组13例,对照组30例。手术适应症情况:肿瘤的持续性增大和神经功能的恶化(12例),肿瘤持续的增大(15例),神经症状的恶化而没有肿瘤生长(1例)。A、B两组及对照组的全部患者中,96.7%均实现了肿瘤全切。任何一组都没有死亡病例。尽管未观察到术后神经缺损或并发症发生率的显着差异,但B组患者出现新发的颅神经功能缺损和CSF漏的风险较高。接受过放疗的患者(A和B组)倾向于在肿瘤床或小脑中发生术后血肿的风险更高。先前未接受治疗的患者的面部神经解剖保存率较高(93.3%),而在A组和B组中分别降至86.7%和61.5%。面神经功能保留率被发现与先前的治疗有关,在对照组为87%,A组为78%和B组为68%。结论:放疗失败后,显微手术可以成功全切肿瘤。然而,术后功能结果往往比未经治疗的患者差。先前有过放疗及部分切除的患者,手术较具挑战性,且预后差。
OBJECT: An increasing number of patients with vestibular schwannomas (VSs) are being treated with radiosurgery. Treatment failure or secondary regrowth after radiosurgery, however, has been observed in 2%-9% of patients. In large tumors that compress the brainstem and in patients who experience rapid neurological deterioration, surgical removal is the only reasonable management option. METHODS: The authors evaluated the relevance of previous radiosurgery for the outcome of surgery in a series of 28 patients with VS. The cohort was further subdivided into Group A (radiosurgery prior to surgery) and Group B (partial tumor removal followed by radiosurgery prior to current surgery). The functional and general outcomes in these 2 groups were compared with those in a control group (no previous treatment, matched characteristics). RESULTS: There were 15 patients in Group A, 13 in Group B, and 30 in the control group. The indications for surgery were sustained tumor enlargement and progression of neurological symptoms in 12 patients, sustained tumor enlargement in 15 patients, and worsening of neurological symptoms without evidence of tumor growth in 1 patient. Total tumor removal was achieved in all patients in Groups A and B and in 96.7% of those in the control group. There were no deaths in any group. Although no significant differences in the neurological morbidity or complication rates after surgery were noted, the risk of new cranial nerve deficits and CSF leakage was highest in patients in Group B. Patients who underwent previous radiosurgical treatment (Groups A and B) tended to be at higher risk of developing postoperative hematomas in the tumor bed or cerebellum. The rate of facial nerve anatomical preservation was highest in those patients who were not treated previously (93.3%) and decreased to 86.7% in the patients in Group A and to 61.5% in those in Group B. Facial nerve function at follow-up was found to correlate to the previous treatment; excellent or good function was seen in 87% of the patients from the control group, 78% of those in Group A, and 68% of those in Group B. CONCLUSIONS: Complete microsurgical removal of VSs after failed radiosurgery is possible with an acceptable morbidity rate. The functional outcome, however, tends to be worse than in nontreated patients. Surgery after previous partial tumor removal and radiosurgery is most challenging and related to worse outcome.
5. 听神经瘤伴瘤周水肿的手术
Surgery of Vestibular Schwannomas with Peritumoral Edema
脑膜瘤中肿瘤周围水肿的存在与手术的复杂性和预后有关,其在听神经瘤(VS)中的意义尚未得到系统评估。方法:对系列患者进行回顾性研究,将VS瘤周水肿与以下因素进行相关性分析:肿瘤影像学特征、手术难度、肿瘤粘连、血管分布、包膜存在、功能预后和并发症发生率。将实验组结果与没有肿周水肿的对照组进行比较。结果:共有30例患者(30/605例患者或5%)出现肿瘤周围水肿。具有瘤周水肿患者更经常发生耳鸣和脑积水,这些VS常富血供。手术难度与瘤周水肿没有明显关系,但和肿瘤的蛛网膜包膜相关。 A组的全部患者均实现了完全切除(对照组为97%)。面部神经保留率为97%(原为98%)。两组的功能结局相似。但是,对照组的术后血肿发生率更高(10%vs. 3%)。结论:伴有局灶性瘤周水肿的VS更富血供,应警惕其术后更高的出血风险。但是,以精良的显微手术技术为前提,肿周水肿的存在不会影响肿瘤全切率及术后功能。
Introduction: The presence of peritumoral edema in meningiomas correlates with complexity of surgery and outcome. Its significance in vestibular schwannomas (VS) has not yet been evaluated systematically. Methods: Retrospective study of patients’ series. Correlative analysis of presence of edema to: radiological tumor characteristics, operative difficulty, tumor adhesion, vascularity, presence of capsule, functional outcome, and complication rate. The findings were compared with those in a matched control group without peritumoral edema (group B). Results: A total of 30 patients (30/605 patients or 5%) presented with peritumoral edema. Patients with edema had more frequently tinnitus and hydrocephalus. At surgery these VS were more frequently hypervascular. No major difference in the operative difficulty in patients with/without edema in regards to difficulty of tumor dissection and presence of arachnoid plane was found. Complete resection was achieved in all patients in group A (vs.97% in the control group B); the facial nerve was preserved in 97% (vs.大概率). Functional outcome in both groups was similar. However, the postoperative hemorrhage rate was higher in the current control Group (10 vs. 3%). Conclusion: VS with perifocal edema are more frequently hypervascular. This may lead to a higher rate of postoperative hemorrhages in the tumor bed and should always be considered. With adequate microsurgical technique, however, the presence of peritumoral edema does not influence the rate of complete tumor removal and the functional outcome.
参考文献:
1. Sato Y, Mizutani T, Shimizu K, Freund HJ, Samii M. Retrosigmoid Intradural Suprameatal-Inframeatal Approach for Complete Surgical Removal of a Giant Recurrent Vestibular Schwannoma with Severe Petrous Bone Involvement: Technical Case Report. World Neurosurg. 2018;110:93-8.
2. Samii M, Gerganov V, Samii A. Microsurgery Management of Vestibular Schwannomas in Neurofibromatosis Type 2: Indications and Results. 2008;21:169-75.
3. Samii M, Koerbel A, Safavi-Abbasi S, Di Rocco F, Gharabaghi A. Using an end-to-side interposed sural nerve graft for facial nerve reinforcement after vestibular schwannoma resection. Technical note. Journal of Neurosurgery. 2006;105(6):920-3.
4. Gerganov V, Giordano M, Samii M. Surgical treatment of patients with vestibular schwannomas after failed previous radiosurgery. Journal of Neurosurgery. 2012;116(4):713-20.
5. Gerganov V, Giordano MG, Metwalli H, Samii A, Samii M. Surgery of Vestibular Schwannomas with Peritumoral Edema. Journal of Neurological Surgery Part B: Skull Base. 2014;75(S 02):a064.




